Artificial Spinal Cord Gel Allows Paralyzed Mice To Walk Again
Tags: News
In what may be one of the greatest achievements in medical sciences, a man-made gel injected into the injured locations in the spinal cord of mice has let them walk again. The recovery happened after 4 weeks of the initial injection.
The gel tries to copy the special matrix that usually surrounds cells. As a result, it constructs a type of scaffold that cells can then use to grow. The gel also creates signals that stimulate the regeneration of nerve cells.
The Artificial Gel And Its Constituents
The test was conducted in Chicago’s Northwestern University by Samuel Stupp and his team. The gel is created using tiny units of protein, known as monomers. These tiny units assemble themselves into longer chains, known as supramolecular fibrils when submerged in water.
For the experiment, mice that could not move their hind legs were selected. Then these fibrils were injected into their spinal cords. The fibrils transformed and became gelatinous at the site of injury.
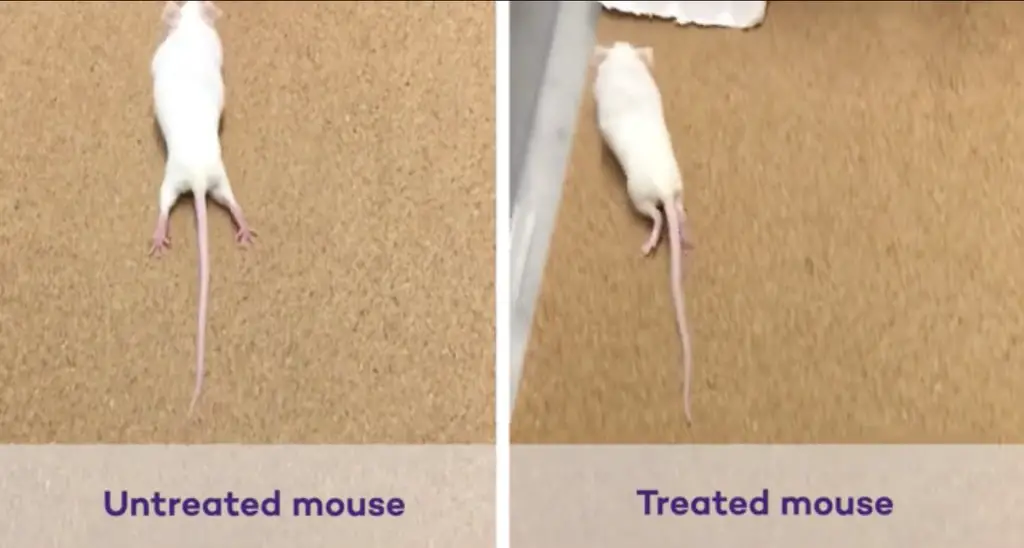
76 mice that were paralyzed were injected with either a fake treatment consisting of a solution of salts or the supramolecular fibrils, 24 hours after the injury took place. They discovered that the artificial gel allowed the paralyzed mice to walk again within 4 weeks following the injection. On the other hand, the mice that were injected with the placebo did not regain any walking ability.
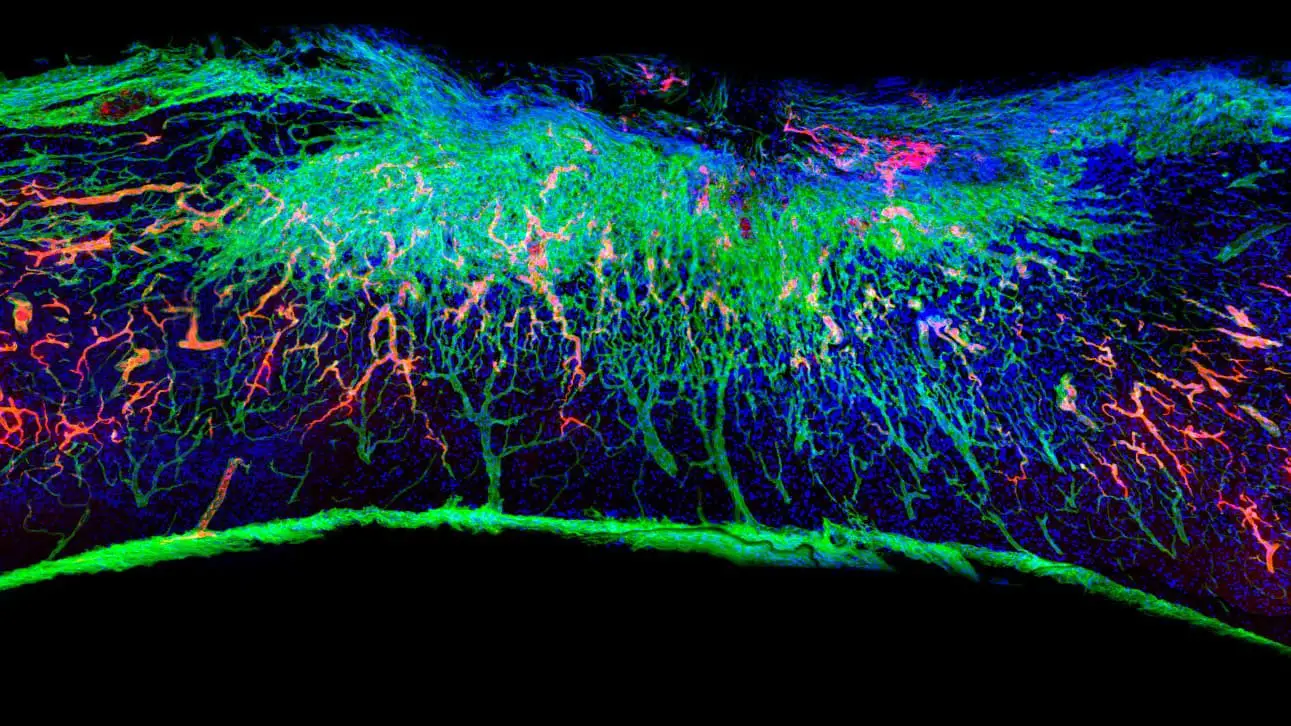
The team discovered that the artificial gel helped in regenerating the ends of neurons that have been severed. Furthermore, the scar tissue present at the site of injury was also reduced in amount by the gel. Scar tissues are the usual barriers that obstruct natural regenerations. The gel was also seen to enhance the growth of blood vessels. This, in turn, allowed more nutrients to be received by the cells in the spinal cord.
Read: Brain-Controlled Robotic Suit Allows A Paralyzed Man To Walk Again
Stupp says that extensive functional recovery, as well as solid evidence of biological repair, was observed by his team. Furthermore, it was a model that comes as close to emulating the same severe injury in humans as possible. Thus, it indicated that this therapy is much better than any other approach.
This is not the only paralysis treatment that is being worked on. Others use proteins, genes, or stem cells. However, Stupp says that their effectiveness and safety are questionable.
The Gel Induces Natural Regeneration.
The mice’s ability to walk was tested using two methods. The mice, at first, were allocated a total score that represented their steps, paw placement, body stability, and ankle movement. The mice that were injected with the gel recorded scores three times as much as the mice treated with the placebo solution.
The second method by which the mice’s walking ability was assessed was by dipping their hind legs in dyes. Then they were allowed to cross a narrow path that had white paper lining it on both sides. This test’s results show that the artificial gel increased the width as well as the length of the stride. Stupp explains that a higher width and length of stride should have a correlation with the more regrown nerve fibers (axons) inside the leg’s muscles.
Read: First Paralyzed Person Treated With Stem Cells Regained His Upper Body Movement
The regenerative effect of the gel is because of short amino acid sequences that are attached at the monomer protein’s ends. The surface of the cells of the spinal cord has receptors that pick up the regenerative signals being produced by these sequences.
However, it is still a long way for the treatment to be feasible for humans. Scaling therapies for mice to that for humans is a humongous task. But experts agree worldwide that if it can be translated to humans, it would be one of the most exciting advancements in human technology.
SUPPORT US ON PATREON AND GET ACCESS TO OTHER EXCLUSIVE CONTENT, CLICK HERE TO LEARN MORE
FOLLOW MIKE ON INSTAGRAM FOR MORE: @MIKESYGULA
Image Credit: (Samuel I Stupp Laboratory/Northwestern University)

Leave Comment: